Lactose intolerance is a syndrome where gastrointestinal symptoms such as abdominal pain, bloating, flatulence and/or diarrhoea manifest in susceptible individuals following lactose intake.1
The Gastroenterological Society of Australia has developed a patient information sheet on lactose intolerance.
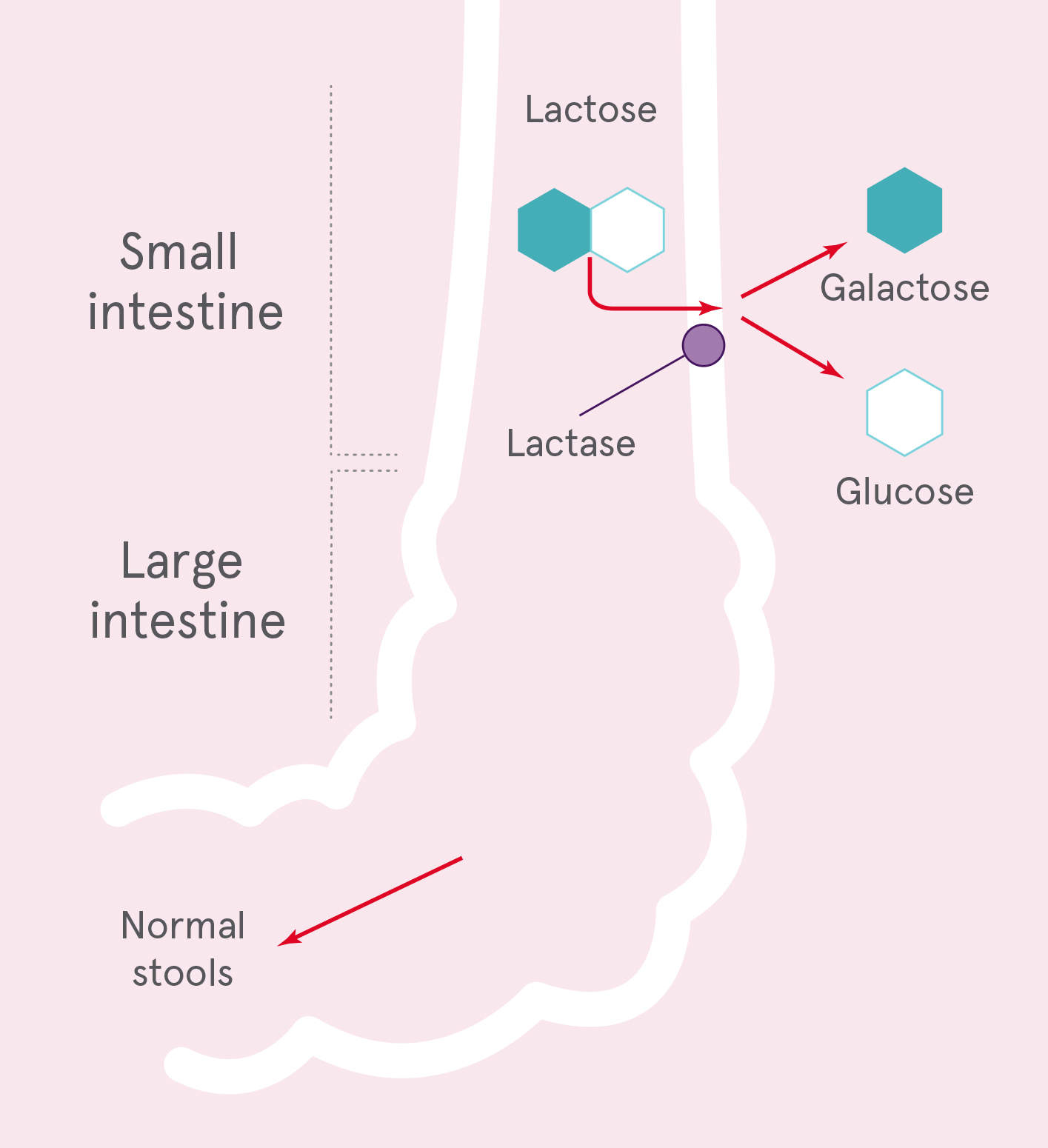
Lactose is the main carbohydrate in milk and milk-derived dairy products and is hydrolysed in the small intestine, by the enzyme lactase, to its constituent monosaccharides (glucose and galactose) which are absorbed readily into the circulation.2 Lactase is a beta-galactosidase that is encoded by the lactase-phlorizin hydrolase gene in epithelial cells lining the small intestine.3 The highest levels of lactase are reported in the infant intestinal villi, but lactase levels subsequently decline in an age-dependent manner.4 In some populations, very low lactase levels follow (lactase non-persistence), but in others lifelong production is reported (lactase persistence). Lactase persistence is reported in people with ancestry from Europe, West Asia, South Asia and parts of East Africa, where milk consumption from cattle, goats and sheep has been a traditional part of the diet.5
Hypolactasia, or decreased lactase enzyme activity, is the commonly cited cause of gastrointestinal symptoms following the intake of lactose containing milk; however, correlation with gastrointestinal symptoms and diagnostic tools for lactase activity is often lacking. For example, a hydrogen breath test will assess lactose absorption capacity, although if low absorptive capacity is demonstrated, this does not necessarily correlate with gastrointestinal symptoms following the intake of lactose-containing milk. For this, a challenge with lactose-containing milk is needed.
Milk digestion sufficient lactase
Milk digestion with hypolactasia
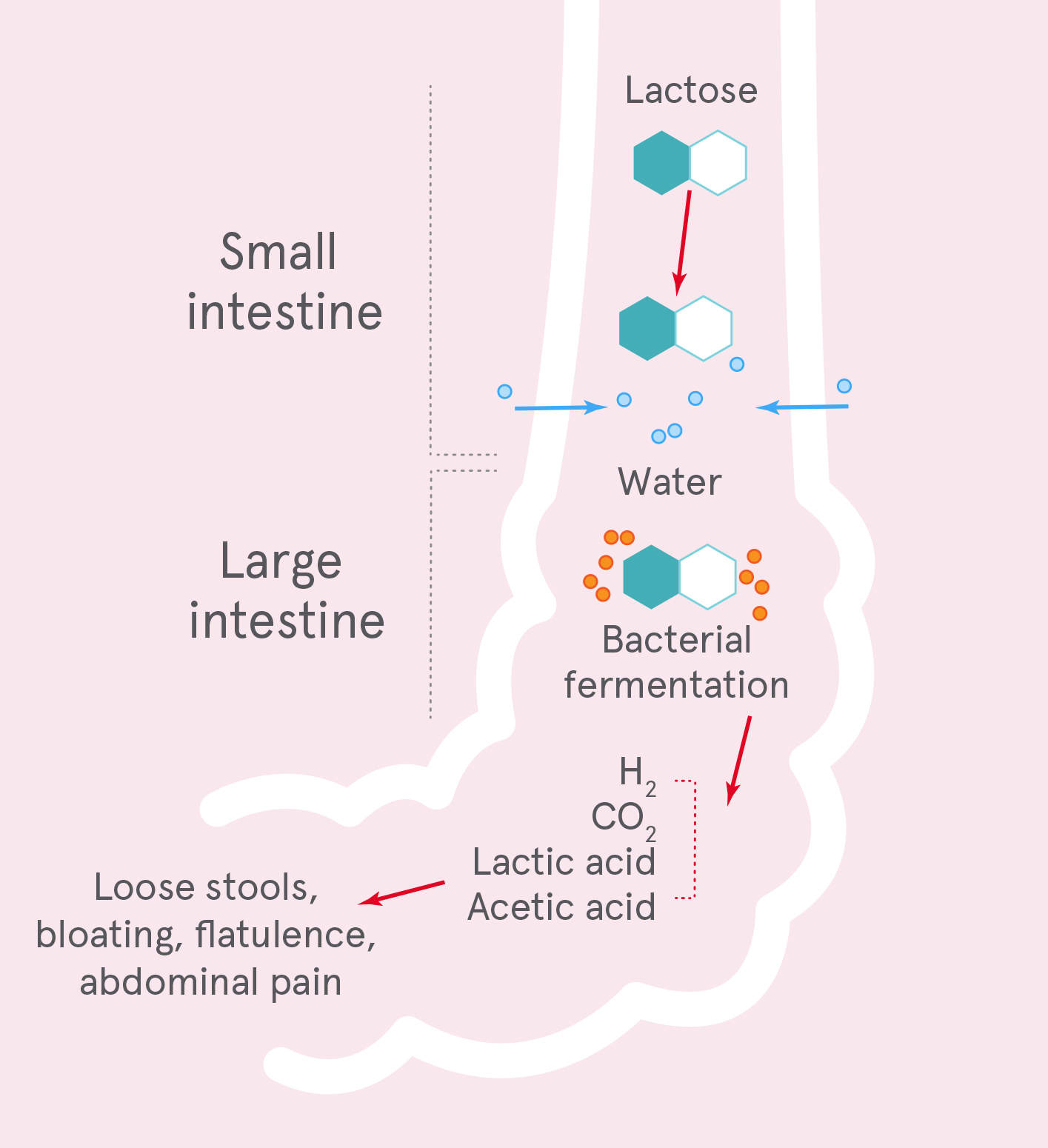
Demonstrated low lactose absorption capacity does not necessarily correlate with gastrointestinal symptoms.6
The National Institutes of Health (2010) consensus statement on lactose intolerance and health states that “many variables determine whether a person who malabsorbs lactose develops symptoms, including the dose of lactose ingested, the residual intestinal lactase activity and individual sensitivity to the products of lactose fermentation”.2 An additional confounder is the wide variation between individuals in both the extent of hypolactasia and the threshold for gastrointestinal symptoms following lactose consumption.7
This variability underscores the National Institutes of Health (2010) conclusion that for lactose intolerance, the “true prevalence is not known”.2
Secondary hypolactasia
Infants, children and adults with lactase persistence may experience secondary hypolactasia in response to gut pathology such as bacterial or viral infection, or cows’ milk protein-induced inflammation, which may cause prolonged or transient reduction in lactase activity.7 Secondary hypolactasia is potentially reversible, and so treatable. Until the underlying cause for secondary hypolactasia is determined and treated, low lactose intake will be required to manage lactose malabsorption gastrointestinal symptoms.
Reduced lactase activity and consequent gastrointestinal symptoms associated with lactose malabsorption can also co-exist with other conditions such as coeliac disease and irritable bowel syndrome, or in children with recurrent abdominal pain.8 In such instances, treatment of the underlying condition is required.
In cases of suspected lactose intolerance, eliminate cows’ and other animal milk lactose until symptoms resolve, then challenge with ~500 mL (2 cups) lactose-containing cows’ milk. It is best consumed in one dose, to assist in identifying the dose associated with the onset of gastrointestinal symptoms. If symptoms reappear, this suggests lactose intolerance.
To distinguish between lactose intolerance symptoms and possible A1 beta-casein intolerance symptoms, see the adverse milk reactions diagnostic algorithm
The next step could be to determine the volume of lactose-containing milk your patient can tolerate before experiencing gastrointestinal symptoms. Start with 50–100 mL (1/5 to 1/3 cup) of lactose-containing milk per day in a single dose and record gastrointestinal symptoms. Gradually increase the daily amount until gastrointestinal symptoms are experienced. The greatest volume ingested without inducing gastrointestinal symptoms is the patient’s tolerance threshold.
